It is believed that the most severe pain is toothache. Although the same can be said about ear pain and headaches. Joint pain is no exception. It can make a person suffer, deprive him of sleep and appetite.
Pain is sharp or dull, stabbing, aching, at night or throughout the day - all these are symptoms of joint diseases.
Prevalence of joint pain
There is no clear pattern between the severity of joint pain and its prevalence. The knee joint may hurt more than the shoulder, elbow and hand at the same time. Sensations in the spine can be painful with widespread osteochondrosis or ankylosing spondylitis. But more often people are bothered by pain in the extremities.
Both arms and legs experience significant stress throughout life - weight, action, injuries. Pain, aches in the joints, and their deformation are inevitable accompanying age-related changes in the musculoskeletal system.
Mechanism of pain

Why joints hurt is a question that even a doctor has a hard time answering unequivocally.
The mechanism of pain when the musculoskeletal system is damaged is quite complex. Most often, these symptoms are caused by the following processes:
- Inflammation of the joints, or polyarthritis.Inflammation itself triggers the production of substances that can cause pain. In addition, they increase the sensitivity of pain receptors to repeated exposure. That is why the usual load on the inflamed joint leads to a sharp pain reaction.
- Swelling of the joint.Its increase in volume looks like a joint tumor. Edema tissues mechanically put pressure on the joint structures, causing discomfort and aggravating the severity of the process.
- Dystrophic changes.This can be called wear and tear of bones and cartilage. With age and constant stress, the function of the joint deteriorates. The production of synovial fluid is disrupted, and the sliding of articular surfaces becomes difficult. Their constant irritation by friction stimulates the growth of subchondral bone. Such marginal bone growths are called osteophytes and can cause real suffering to a person. They look like protruding bumps on the joints. Osteophytes are often injured, and this causes their inflammation, completing the pathological circle.
- Trauma and post-traumatic complications.Serious injuries: bruises, dislocations, fractures do not go away without leaving a trace. Even if the damage is cured, joint pain and stiffness may remain for the rest of your life. Doctors often encounter complaints of aching pain in damaged joints. They usually get worse when the weather changes or at night.
- Exchange disorders.Calcifications are deposited in tendons and ligaments due to metabolic disorders. Their infringement leads to a sharp pain syndrome.
These pathological processes in the joints develop in diseases of the musculoskeletal system.
Diseases of the musculoskeletal system
The number of joint diseases is large. There are rare forms - isolated throughout the world, and there are also those that are found in most people. The prevalence of these diseases explains the fact why every person has joint pain at least occasionally.
It is important to know the main diseases of the musculoskeletal system, so as not to ignore dangerous symptoms, but to begin to treat and cure the disease in time.
Osteoarthritis
Doctors constantly hear from elderly patients that they have pain in the joints of their arms and legs, lower back, and neck. In addition to pain, they complain of joint deformation, difficulty walking, and the inability to do homework.
These symptoms are characteristic of osteoarthritis of the joints. In the case of deformation of bones and cartilage, it is called deforming osteoarthritis. Deforming osteoarthritis in severe form can make a person completely disabled.
Osteoarthritis affects any joint – large and small. It is only important that they experience sufficient stress.
If you overload the joints, osteoarthritis will develop several years earlier, especially if there are predisposing factors. These include:
- Constant load. It can be redundant or monotonous. Static loads play an important role in the development of arthrosis changes.
- Hypothermia or overheating.
- Injuries - bruises and fractures, subluxations and dislocations.
- Excess weight. Fatness is one of the most important risk factors for the development of deforming osteoarthritis.
- Poor nutrition.
- Lack of movement.
- Infections and subsequent inflammation of the joints are polyarthritis.
Degenerative diseases of the shoulder girdle

The shoulder joint is the most mobile joint in the body, with the maximum range of motion. It bears dynamic loads, so degenerative changes in the structures of the shoulder girdle are rare.
They usually develop in old age. Marginal bone growths appear and articular cartilage atrophies. If degenerative changes in the shoulder joint are pronounced, then the cause should be looked for. This usually occurs due to a fracture or osteochondromatosis.
Pain in the shoulder joints is aching and constant; stiffness is often associated with degenerative changes in adjacent structures:
- Deposition of calcifications in the supraspinatus tendon and the resulting painful abduction arc syndrome. With this pathology, pain in the joints occurs when trying to move the shoulder along a certain arc. If you change the angle of inclination, the pain disappears.
- Frozen shoulder syndrome. This condition is characterized by severe stiffness of the shoulder girdle. Occurs as a result of prolonged immobilization of the shoulder - when applying a bandage, providing rest for the arm with thoracic radiculitis.
No pronounced deformation of the elements of the shoulder girdle is observed. Symptoms and complaints associated with damage to adjacent structures, rather than deforming osteoarthritis of the shoulder, usually come first.
Osteoarthritis of the elbow joint
The likelihood of developing degenerative changes in the elbow joint is low. It increases in old age and in persons engaged in certain professions. Monotonous physical activity has a negative impact on joint processes, especially when exposed to vibration.
Deforming osteoarthritis of the elbow region is often found in tennis players, masons and miners, blacksmiths, and foundry workers.
Usually the pain in the joints is dull, aching, and intensifies with exercise. No significant deformation of the joints is observed. Sometimes, under the influence of provoking factors, inflammation of the joints also joins osteoarthritis, a painful swelling occurs in the elbow area, and the pain bothers you even at rest.
Deforming osteoarthritis of the hands and joints of the fingers
In recent years, the diagnosis of osteoarthritis of the hands has become the answer to the question of why finger joints hurt at a young age. This disease is rapidly getting younger. Already at 30–35 years of age, with complaints of pain in the joints of the fingers, signs of the first degree of deforming osteoarthritis can be seen on an x-ray. The reasons for this are varied:
- The number of professions that place stress on the joints of the hands and fingers is increasing - programmers, typists, and simply active computer users. And mostly young people are involved in this.
- Working in hypothermic conditions. These are drivers of trams and trolleybuses in winter, builders, and villagers.
- Lack of normal dynamic loads on the finger joints. Few people strive to do gymnastics, especially therapeutic exercises.
- Concomitant diseases - inflammation of the joints.
The joints of the fingers and hands become deformed over time, and an inflammatory tumor can be detected in the area of the phalanges with the development of polyarthritis. Movements in them become painful and difficult. Joint pain is intermittent at first, but then changes to constant, dull or aching.
Degenerative foot diseases
The joints of the legs are more susceptible to degeneration, since their main load is static. Weight and static loads are the main causes of the development of deforming osteoarthritis of the legs. In this area it occurs in the following forms:
- Damage to the hip joints – coxarthrosis.
- Damage to the knees with the formation of gonarthrosis.
- Dystrophic diseases of the foot.
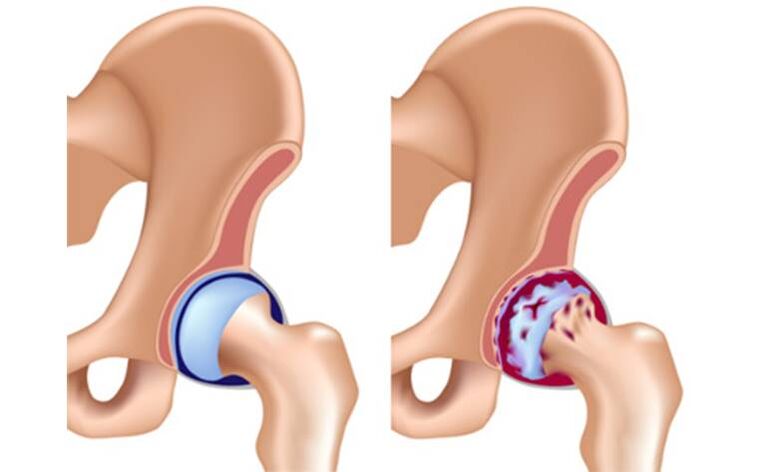
Coxarthrosis
Coxarthrosis is a common and dangerous disease. Initially, a person pays attention to symptoms such as pain in the joints, crunching, clicking when walking. All this is temporary and does not greatly affect the quality of life. As the disease progresses, stiffness worsens, and difficulty appears when trying to abduct or adduct the leg.
Joint pain can be excruciating, debilitating, and bother you at any time of the day. In the mornings, my movements are constrained, I have to do exercises for the hip joints in order to move apart.
Gonarthrosis

Throughout life, the knees experience loads that significantly exceed a person’s weight. This inevitably leads to the development of degenerative processes in them. If a person suffers from obesity of at least the first or second degree, deformation of the knees will occur much faster. In grades three and four, deforming osteoarthritis is more likely to develop at a young age.
Osteoarthritis of the knee joints has its own characteristics. Why does joint pain so often occur in this area? In addition to the proliferation of bone spines and cartilage degeneration, calcium crystals are deposited in the joint cavity. A kind of depot of calcifications is formed. This disease is called calcium pyrophosphate crystal deposition.
At first they can be found only in the thickness of the cartilage, then on its surface, in the articular cavity, tendons and even muscles.
Deposition of calcium crystals worsens the course of deforming osteoarthritis. The disease manifests itself as aching pain, which can turn into acute pain when the calcification is pinched. The mobility of the legs is significantly limited. In the area of the knees, deformed articular surfaces, bone growths are visible, and dense nodules can be palpated.
Dystrophic changes in the joints of the feet

The joints of the feet are less susceptible to deforming osteoarthritis. An exception is the metacarpophalangeal joint of the first toe. Its deformities occur in almost every person after 55–60 years. In women, it becomes deformed at an earlier age. The reasons for this are the abuse of narrow, uncomfortable shoes with heels.
In addition to the inconvenience and unaesthetic appearance of a deformed finger, a person experiences severe pain in the joints. As osteophytes grow, protruding bones form around the toe, making it difficult to wear even the widest shoes. Constant injuries to osteophytes cause inflammation of the joints of the toes - polyarthritis develops. The situation can be complicated by the addition of an infection.
Inflammatory diseases of the musculoskeletal system

Inflammation of the joints, affecting several groups of joints at the same time, is called polyarthritis. If only one joint is inflamed, this form will be called monoarthritis. Symptoms will depend on the type of inflammation or infection that caused it:
- Joint pain.It is often acute - burning or shooting. If the cause of arthritis is an infection, the inflammation becomes purulent. In this case, the pain will be throbbing and very strong. In chronic and subacute forms, joint pain will resemble the variant with arthrosis.
- Changing shape.In an acute process, an inflammatory tumor forms in the articulation area, the skin color changes, and the temperature rises. If a bacterial infection occurs, general symptoms of intoxication appear - high fever, chills, and health deteriorates sharply. The disease is especially difficult to tolerate in cases of polyarthritis.
- Impaired function.Movement in an inflamed joint is significantly limited due to pain and fluid accumulation in the joint cavity. This swelling, like an inflammatory tumor, mechanically prevents movement.
Causes of arthritis
The causes of arthritis are varied. These diseases are usually divided into main groups:
- Infectious.They develop when the joint is directly affected by an infection, such as Lyme disease. The infection can be viral or bacterial, penetrate from the outside or from an affected neighboring organ, bone. Arthritis caused by bacterial infection is especially severe.
- Reactive.In this case, the inflammatory process develops as a reaction to an infection in the past or present. These include damage to the musculoskeletal system after influenza, colds, and urogenital infections. An important sign is the connection with infection.
- Autoimmune.Sometimes a person’s immune system begins to destroy its own cells. The manifestations of such diseases are varied, but articular syndrome is usually most clearly expressed. The most common autoimmune pathology is rheumatoid polyarthritis. It is characterized by severe deformation of the joints with persistent pain.
Autoimmune polyarthritis cannot be cured, but it must be stopped in order to keep the disease at an early stage.
Treatment of joint diseases

What to do if you are diagnosed with a joint disease? Do I need to take medications, antibiotics, or can I limit myself to folk remedies? Only a doctor can correctly answer all questions, and he will prescribe the appropriate treatment.
ethnoscience
Folk remedies have been prescribed for a long time - both by healers and modern doctors. They are quite capable of relieving inflammation and eliminating pain, reducing swelling in the affected area.
Among folk remedies, cabbage leaf is considered the undisputed leader. Applying it cold or in a compress with honey to a sore joint can relieve inflammatory manifestations and alleviate the condition. Plantain leaves, chopped mushrooms, and vodka liqueurs are also used.
The arsenal of folk remedies is varied, but you need to remember that they can only treat mild forms of diseases and always under the supervision of a doctor.
Medicines

Medications used in the treatment of joint diseases are aimed at all parts of the pathological process. Main groups of drugs:
- Analgesics and anti-inflammatory drugs.Usually these are drugs from the same group. Since the main symptom of joint diseases is pain, relieving it is the doctor’s first priority. A good effect is achieved when using local remedies.
- Steroid hormones and cytostatics.It is strictly forbidden to take these medications without a doctor's prescription. They are used for all serious autoimmune processes and are designed to relieve specific inflammation in the body. Without hormonal drugs, it is impossible to get rid of the pain and inflammatory tumor in rheumatoid polyarthritis. They also inhibit joint deformations.
- Antibiotics.They are prescribed if the cause of arthritis is a bacterial infection. Broad-spectrum antibiotics are used that penetrate well into bone tissue. Sometimes, if the pathogen is persistent, the doctor may treat the infection using several groups of antibiotics. This is also justified if the disease is caused by a mixed infection. It is necessary to remember that antibiotics are strong drugs with individual side effects, and strictly follow the doctor’s instructions during the treatment process.
- Preparations that protect and restore cartilage.It is impossible to treat chronic polyarthritis and deforming osteoarthritis without chondroprotectors. For this purpose, both single drugs - chondroitin or glucosamine - and combined ones are used. There is an extensive evidence base on the use of chondroprotectors based on many clinical trials.
- Intra-articular injections.This is the best way to deliver the drug directly to the site of the disease. Typically, hormonal anti-inflammatory drugs are injected into the joint cavity. In recent years, hyaluronic acid has also been used for intra-articular injection.
Physiotherapy

It is not worth treating joint diseases only with medications. The integrated use of physiotherapeutic techniques (magnetotherapy, electrophoresis) and physical therapy significantly increases the chances of recovery.
Orthopedic devices are also used to limit movement in the affected joints. These include orthoses and splints. The purpose of these devices is to reduce the load on the diseased joint.
Surgical treatment
A radical cure for advanced osteoarthritis is endoprosthetics. Only this method is capable of replacing a destroyed joint with a synthetic one, restoring its full range of motion.
Endoprosthesis replacement is a treatment option in situations where conservative therapy is powerless.































